Vitamin K is a fat-soluble nutrient involved in the production of various proteins. These proteins are the precursors and building blocks for pathways that regulate blood clotting, bone formation, and calcification of the arteries. In other words, it’s pretty important.
I’m always curious why we call things certain names, so here’s an interesting factoid about Vitamin K: it was named because it was discovered in Germany for its role in coagulation. Coagulation in German is Koagulation.
Vitamin K, much like Vitamin D or B, isn’t one thing. Instead, Vitamin K is an umbrella term given to a family of similar compounds. There are two major types of naturally occuring Vitamin K – Vitamin K1 and Vitamin K2. There are synthetic forms of Vitamin K: Vitamin K3, K4, and K5. We only mention these here for completeness. Vitamin K3 was removed from the market for being potentially toxic in high doses.
Let’s explore Vitamin K1 and K2 and figure out which, if either, is a good idea to supplement.
Vitamin K1
Vitamin K1 is called phylloquinone (I won’t use the chemical names again because my eyes go cross trying to type them). Vitamin K1 is found in plants, especially leafy greens, as Vitamin K aids in photosynthesis. As you can see, kale and friends have a bucketful of Vitamin K compared to other foods:

Vitamin K1 is the main dietary form of Vitamin K, outnumbering Vitamin K2 10 to 1. The thing to know (that I’ll repeat ad nauseum) about Vitamin K-rich foods is absorption from food sources is poor since Vitamin K is tightly bound to chloroplasts (cells used in photosynthesis).
Vitamin K is well absorbed in the free form – the form found in supplements. The NIH cites a study that compared absorption of Vitamin K from spinach to a tablet. It was found only 4-17% of the dose was absorbed from spinach when similar amounts were ingested. That’s pretty low number and a big range. When Vitamin K1 is in supplements, the absorption is over 80%.
There hasn’t been any Recommended Daily Allowances set for Vitamin K intake based on a lack of evidence. Instead, an Adequate Intake level has been established.
These numbers are here:
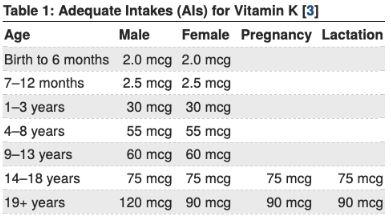
Most of us reading this article will need 90 mcg or more a day per the established recommendations.
“Bro, I’m going to eat ½ cup of kale and be good for 6 days” says the surfer who can do quick math. First, the Adequate Intake levels are technically low estimates of what people need for basic functioning. There’s probably good reason that people get a little more. I’m not advocating mega-doses, but it is quite possible these numbers are a minimal goal.
Second, absorption from food is low and erratic, bro. Don’t think “one and done” with Vitamin K-rich foods; because of poor absorption of Vitamin K from food, it’s a really good idea to eat lots of servings of varied Vitamin K-rich foods to guarantee crushing your daily K goals.
“How do I know if I get enough Vitamin K, brah?” says the more humble surfer dude. We don’t have an easy way to assess Vitamin K status. We basically only know if you have a Vitamin K problem if you’re bleeding irregularly. We check indirectly, by seeing if you bleed longer than normal, then wack you with a dose of Vitamin K to see if that fixes the problem. Therefore, it isn’t routinely checked, nor is it indicative of “optimal” Vitamin K status, just deficiency.
For everyone between the bleeder and the #KaleKommanders, we are flying blind. We know pretty reasonably what we are ingesting, based on estimates of content in food like the tables above. How I read this whole thing is, while we may be consuming 120 mcg (an amount at or over the AI), on average, we are not absorbing much of that. Many of us may be not getting enough Vitamin K, which can contribute to suboptimal health in Vitamin K-related body systems.
I can’t stress it enough! If we estimate a 10% absorption from food, we need to ingest over 900 mcg of Vitamin K from kale, spinach, collards, etc etc. That’s a lot of servings, especially for many of us who don’t do a great job with greens daily. Vitamin K supplementation, whether on its own or in a multivitamin, may be a good idea if our diet isn’t rich in dark, leafy greens.
Vitamin K2
Vitamin K2 is called menaquinone. Vitamin K2 is made almost exclusively by bacteria converting Vitamin K1. As such, Vitamin K2 is found predominantly in animal products: eggs, dairy, meat, or fermented foods like cheese or yogurt. The only problem: there’s not much of Vitamin K2 in these foods, especially when compared to the Vitamin K1 content of common foods.
Vitamin K2 itself is a group of compounds, not a single thing. You may have heard of these… MK-4 and MK-7 are two such types. They abbreviate as MK-n, where M is for menaquinone, K is for Vitamin K, and n is for the length of the “tail” of the compound. The higher the number, the longer the “tail” and the larger the compound.
Vitamin K2 compounds go from MK-2 all the way to MK-13. We really only care about the MK-4 and MK-7 forms, as they have the most research.
MK-4 is special because many animals can make it without bacteria. Bacteria, though, are the ones responsible for making those tails longer, taking MK-4 and smaller and turning them into the MK-5 and larger. The gut flora have a role in converting dietary K1 into K2, and people on high dose antibiotics can have a Vitamin K deficiency. All the more reason to use a well made probiotic!
While Vitamin K2 can be found in foods, it is in very short supply. In fact, the only food rich in Vitamin K2 is natto, a Japanese food made from fermented soybeans. Here’s a short list of Vitamin K2 rich foods:
- Natto, 3 ounces – 850 mcg of MK-7
- Chicken breast, 3 ounces – 13 mcg of MK-7
- Mozzarella Cheese, 1.5 ounces – 2 mcg of MK-4
Unlike Vitamin K1, Vitamin K2 from foods has good absorption.
Is one form of Vitamin K2 better than another K2? There’s some data that says MK-4 is better for this thing and MK-7 is better for that thing. There’s little evidence to prove one is conclusively better than the other. If you choose either MK-4 or MK-7 over any of the other forms of Vitamin K2, you’re going to be more than fine. MK-7 is my pick, as it has a long half life, meaning it hangs around the body a bit longer.
The best question to ask is, “Which is better, Vitamin K1 or K2?”
Vitamin K1 vs K2
We get about 10 times the amount of Vitamin K1 in our diets than we do K2. Does that mean it is the better option for us? Maybe not.
The first step in comparing Vitamin K forms is to ensure consistency. Since the absorption of K1 is so erratic, the only way we can study the differences is to use supplements in addition to a consistent dietary intake, whether that intake is a lot or none.
When we look broadly, both Vitamin K1 and Vitamin K2 will get the results we’d hope and expect. The difference is in their efficiency.
There are numerous observational studies that show Vitamin K2 has a more profound impact on the body, and quicker, than Vitamin K1. For example, one study showed MK-4 had some impact on blood vessel calcification where K1 did not.
Based on the small pool of decent literature around Vitamin K1 vs K2, I lean towards K2 as the choice for Vitamin K supplements, but the differences may come out in the wash when we study further. To further support my “either or” position on it, our Vitamin K supplements use MK-7, while Calcium Care uses spinach, rich in Vitamin K1.
Vitamin K’s Role In The Body
As we started the article off we mentioned Vitamin K creates proteins that are used in essential processes that control blood clotting, bone formation, and hardening of the arteries. I’m not going to get full nerd on you in this one, but I’m going to address some common misconceptions in each area to ensure you are informed around these industry talking points.
Vitamin K and Blood Coagulation
The effect on blood is what Vitamin K is probably most known for. Warfarin, an anticoagulant or “blood thinner”, reduces the amount of active Vitamin K. As a result, some of the factors our bodies use to make clots aren’t formed. The end result – less clotting, more bleeding.
People on warfarin can’t eat Vitamin K rich foods as it would be kinda counterproductive. The real secret is this: consistency matters more than abstinence. Talk about sentences that shouldn’t be taken out of context! Let me clarify…
Most practitioners would recommend avoiding Vitamin K rich foods while on warfarin because it is the BEST way to guarantee consistency around the activity of warfarin. Your warfarin dose will remain the same because the intake of Vitamin K will be so low. If you eat a kale smoothie every day, your warfarin dose would need to be adjusted (normally up) to make up for the added Vitamin K you’re eating. See the relationship?
Some doctors will work closely with really engaged patients, allowing a consistent Vitamin K food intake. Unlike marijuana prohibition, these doctors are all for the green!
It’s a problem, though, when one day you eat like a rabbit and the next like a viking. The amount of warfarin needed to overcome the changing Vitamin K levels would change day to day, making it difficult to get a consistent level to prevent clots. Clots are way worse than skipping spinach. If you eat a little bit like a rabbit every single day, your Vitamin K intake will remain consistent and your medicine can be adjusted to that intake.
With all that said: do not change a thing about your diet if you are on warfarin without speaking to your doctor first!
Other anti-clotting medicines don’t work on the Vitamin K pathways, therefore have all the spinach you want.
Reduced Vitamin K and increased bleeding is a great thing if someone is at risk for creating clots that could potentially kill them. It’s not so great if you just want to get your Wednesday going. Low dietary Vitamin K can lead to this same endpoint – increased risk of bruising, bleeding, and longer time to create clots. This requires a DEEP deficiency at a consistent rate. Not the “I don’t eat salads 3 times a day” deficiency stuff. Most of us don’t have to worry.
A bit of misinformation I must clarify: MK-7 and Vitamin K2 is NOT ok with warfarin. Some “experts” have advised customers that K1 and K2 are different when it comes to warfarin, but the literature says otherwise.
A common question I get asked is, “If I take too much Vitamin K and I’m not on warfarin, will I be at a higher risk of clotting?” This is a good question as it shows you are thinking about the relationship! Extra Vitamin K does NOT increase bleeding risk, and we’ve tested doses 1000 times what most of us will eat.
Vitamin K and Bone Health
Vitamin K has a role in formation of osteocalcin. It has both osteo- and –calcin in the name, so it must be about bone building, right?
Sort of. Osteocalcin does not directly build bones. It is a compound made by cells that build bones. Osteocalcin is actually a hormone that has roles in numerous body systems: the pancreas/insulin, testes/testosterone, and even the muscles. Osteocalcin is a secondary marker or measure of bone formation. We can use osteocalcin to determine if your bone-building medicine is working. If the cells that build bones are active, that means there is more osteocalcin.
As it relates to our current discussion, active bones need good levels of Vitamin K to keep the osteocalcin churning. If your Vitamin K is low (which it probably is if you don’t eat your veggies!), osteocalcin will be there, but may be useless for the body.
Low dietary Vitamin K is associated with poor bone mineral density. Improving Vitamin K intake improves bone mineral density in people who have bone problems because of low Vitamin K intake.
Just because that relationship exists, doesn’t mean the inverse is automatically true. Extra dietary Vitamin K will not do anything for bone mineral density.
Let me rephrase for accuracy: current evidence leans towards Vitamin K supplements and excess dietary intake may have some positive effects on bones, but not enough to change any outcomes (aka fractures). Extra Vitamin K, in small studies, has positive impact on some other markers of bone health, but does not change overall bone density or fracture risk. More studies with better methods are needed.
Taking Vitamin K ensures you will not have weakened bones because of a Vitamin K deficiency. There is a relationship between adequate Vitamin K intake and normal bone health. Some of us aren’t getting enough Vitamin K, so here’s your nudge to get more.
“BUT BUT BUT Vitamin K is a prescription drug for osteoporosis in Japan!” Why yes, it is. I’ve included a chart with a comprehensive listing of Vitamin K studies on bone health, and how most of them show a net positive.
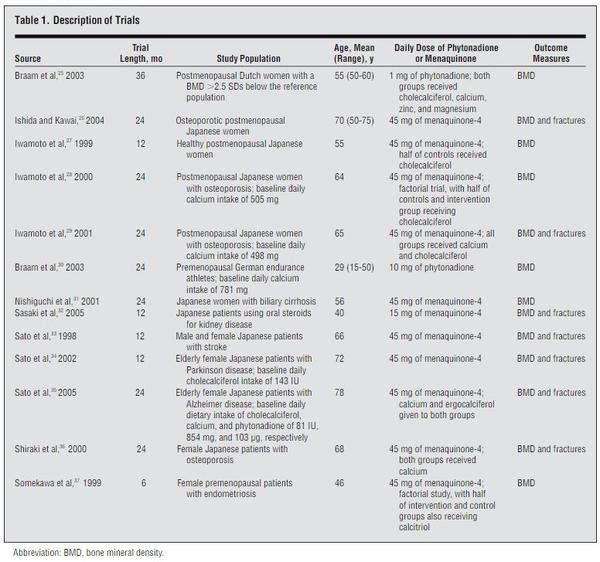
Having access to data like this is truly awesome. Scientific rigor around a nutrient and even the most conservative doc could say, “Let’s try it!”
When I read this chart, do you know what note I marked up on the image after I saved it for this article? I wrote:
DECEPTION
Look again at that far right column at the studied doses. What do you see? 1, 10, and 45? Many people would look at that and say, “OK, I need my Vitamin K to be 45.” And how lucky we are that the doses available are 45, 90, and even 120.
The problem is the doses that were studied were 45 milligrams, and our supplements and recommended intake numbers are in micrograms. That is a 1000x difference.
Here’s what I hypothesize: Supplement manufacturers use those doses in part to confuse consumers who are not trained to pay attention to those details. Why else would we chose those numbers? Why not 60 or 100? If our average intake is 66, why not 70? Yes, the recommended Adequate Intake of Vitamin K numbers are 90 or 120, but there are very few vitamins whose traditional doses align with the RDA numbers.
The doses of Vitamin K that have had any net change on bone health are 1000x dietary intake recommendations and supplement doses. Don’t be fooled into thinking using VItamin K supplements will have a positive impact on your risk for fractures.
What Vitamin K will definitely do is ensure you will not have any bone weakness due to too low Vitamin K. Possibly there are some positive effects on the bone getting a little extra Vitamin K. So supplement Vitamin K after you try your darndest to get it from your diet. I just want consumers to be informed and have reasonable expectations of what exactly Vitamin K will do for your bones.
Vitamin K and Blood Vessel Calcification
Another protein Vitamin K helps make is something called MGP, which prevents blood vessel hardening. This, to me, is the most interesting part of Vitamin K intake. In people who don’t get enough Vitamin K, they have less MGP and more calcification of their blood vessels, which can lead to clogged arteries, strokes, and heart attacks.
If I get extra Vitamin K, will I have pillowy soft blood vessels that move like a waterbed? Kinda sorta maybe.
Some small studies have shown a connection between low dose supplementation and levels of vasculature hardening. Less calcification is seen, but we don’t know if that really matters.We have no studies done in a big way, nor do we have data showing that Vitamin K will prevent heart disease. Much like with Vitamin K and bones, any little thing we can do to help, we should do it. Especially since the “cost” is so low. Hardening of the arteries is a bit more serious for most of us than a risk of fracture, so eat that broccoli.
The Vitamin K and Vitamin D Connection
There’s a unique, dynamic, and complex interaction between Vitamin D and Vitamin K. It’s a brilliantly coordinated dance; it’s a venerable tango of interlocked destinies that climaxes in nothing short of magic.
Without further ado, the connection:
- Vitamin D helps bones
- Vitamin K helps bones
Phenomenal, right?

If you’re new to my writing, that was sarcasm. The natural products industry wants to markup their Vitamin K and Vitamin D products, so they combine them and tell you they’re magical together. While they’re both important for bone health, the two together isn’t some fate-filled connection that we’ve been missing for 200+ years.
Take your Vitamin D. Use Vitamin K if you’d like. But there is no reason to take them at the same time. Vitamin D3 doesn’t even need to be taken every day based on how it interacts with our bodies. What matters most is getting the right forms and the right doses, not taking them in some magical combo pill.
You also technically don’t NEED both for your bones to be healthy. You can take one without the other; both will benefit you individually. I believe a comprehensive bone health regimen is important, meaning calcium, Vitamin D, magnesium, boron, collagen, silica, and more. As we said in Calcium Doesn’t Work after a certain age, proper nutrition will support the current status of your bones but has minimal impact on making them new again.
My Vitamin K Recommendations
“Let your food be your medicine” is a mantra I’ve spouted for most of my practicing years and others have said in one form or another for generations. When it comes to Vitamin K, I recommend eating a diet rich with varied sources: kale, spinach, broccoli, and natto are great places to start. We absorb only a small amount of Vitamin K from our foods, so it is prudent to have many servings of these healthy foods daily.
There’s a good chance we’re not getting enough Vitamin K. Our diets aren’t great, plus there is poor dietary absorption of Vitamin K. We don’t frequently assess Vitamin K levels unless there is a problem, so we’re flying blind.
Vitamin K has a role in coagulation, bone formation, and calcification of the arteries. If we don’t get enough Vitamin K, we WILL have problems. If we get enough, those problems almost entirely go away. There is some positive signs of a little extra Vitamin K may do good things for bones and blood vessels, but nothing we should be mega-dosing for or changing our lives over.
To ensure intake above the adequate intake standards that are currently set (that themselves may be on the lower side), using supplemented Vitamin K may be wise. Supplemented Vitamin K has much better absorption than food, and MK-7 seems to stick around longer in the body than Vitamin K1.
Doses supplemented at 45, 90, or even 120mcg will have no overdose risk or side effects but guarantee enough intake to prevent serious long term problems.
Little risk. Low cost. Possible reward. I’m all for Vitamin K supplementation.
Strip Away The Hype And You Still Are Alright
Don’t believe the hype around Vitamin K and osteoporosis. The doses we’d get from supplements are FAR below doses that have had an impact on bone density and fractures. Dietary Vitamin K does have some impact on markers of bone health, even those with osteoporosis, but extra dietary Vitamin K will not rebuild weakened bones.
Pull away all the fake promises, Vitamin K is still great and should be a part of your regimen. Vitamin-K rich foods are a part of our Vital 5 recommendations, so we’ve always beat this drum loudly.
The natural products industry banks on consumers understanding the loose connections between nutrient and disease. The misconception lines their pocket at your expense.
Thankfully though, you’ve got a big mouth pharmacist helping you along the way. 🙂
Just trying to keep it real…

Neal Smoller, PharmD
Owner, Pharmacist, Big Mouth