A topic has been coming up with alarming frequency at the store this week: reflux. Many people are suffering from it. Everyone hates the medicine.
Acid reflux isn’t fun to live with. Heartburn, taste changes, tongue swelling, and a general nauseous… has anyone looked at the quality of their day and decided they needed any of that?
The pendulum now swings away from medication towards natural alternatives. This is fine, but there are a few points that must be understood about the medicine for reflux, about reflux itself, and about natural remedies for reflux that must be considered before we make any major moves.
Much like our conversation around flu shots, avoiding medication is fine if you are doing so because you want to and you are an adult. It is not fine, in my honest opinion, if it is based on misinformation or misunderstanding about the risks of traditional therapy or an exaggeration of the benefits of natural treatment. Let’s get ranty about all of it.
Acid Reflux
Acid reflux is caused by stomach acid and digestive enzymes creeping up into the esophagus instead of staying where it is told. See my very accurate drawing:
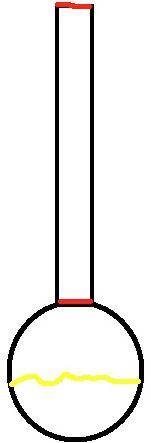
No, this is not a bong you pick up at one of the head shops here in Woodstock. That is a Neal drawing of your esophagus and stomach. The red areas are sphincters – natural plugs that are supposed to allow food down and block stuff from coming back up.
Reflux happens when the acid and fluids from the gut move up into the esophagus. Over time, this is called GERD (gastroesophageal reflux disease) and can lead to serious problems.
The long-term exposure to acid can erode protective factors on the esophagus, which then causes the esophageal cells to change to pre-cancerous cells (Barrett’s esophagus).
This then can lead directly to cancer of the esophagus and that is just not fun. There is a spectrum of diseases and conditions that can both cause this and result from reflux, but we will keep the conversation nice and simple here.
Reflux happens typically because of a weakening of the lower sphincter (LES) or an overproduction of acid. When you have the spilling of acid upwards, lots of unpleasant symptoms happen.
Heartburn is the most common, where the harsh acids cause a physical pain in the esophagus and it radiates outwards in the throat and mid-chest. If you are like me, you’ll get frequent coughing.
My poor classmates in college always wondered why I was constantly clearing my throat during lecture: it was acid reflux.
Acid spilling upwards into the upper respiratory tract (back of the throat and mouth) can cause taste changes, tongue swelling, and can even trigger asthma symptoms and cause congestion in some people.
I consider people who have symptoms, though unpleasant, lucky. Many people have silent reflux and go asymptomatic. This is more dangerous, as the acid exposure over time can cause serious complications – the most serious being esophageal cancer.
Some people like to blame low acid for reflux symptoms. While hypochlorhydria (low acid) is a real thing, the only people that seem to be talking about it seriously are natural health blogs.
Risk Factors For Reflux
Not everyone gets reflux. Typically reflux comes once-in-a-while, usually due to overeating or eating “trigger” foods. Over time, our bad habits will lead to reflux happening on a more regular basis. Here are some risk factors for getting reflux:
- Eating high-fat meals – fat sits in your belly for a while. We recommend small amounts of good fats to build your campfire because it burns slowly. Eat too much, however, and the contents of the stomach just sit there while it digests. It eventually backs up and reflux happens.
- Eating large meals – stretch out your gut with a Thanksgiving level meal and it will fill to the brim, making it really easy for the acid to head north.
- Sitting or lying after eating (this includes eating right before bed) – gravity will pull the liquid contents of the stomach up.
- Standing while you eat – along the same lines, if you are standing, you’ll probably be leaning over frequently causing gravity to go to work.
- Not chewing your darn food – this is why I have reflux. Working retail, looking for that dopamine surge after eating a tasty food, or just being in a mindless rush means I chomp chomp swallow. Digestion starts in the mouth, so a slow chew of the food is essential to break down enzymatically and physically, allowing food to pass gently over the upper sphincter, keeping it intact.
- Smoking
- Alcohol intake
- Caffeine
- Eating certain foods (see the next section for a complete list).
- Stress
Foods that Trigger Acid Reflux
If you have reflux, you should do your best to avoid any and all trigger foods.
- Alcohol
- Red Wine
- Chocolate
- Peppermint
- Tomatoes
- Coffee
- Caffeinated drinks
- Carbonated beverages
- Chocolate (Yes, chocolate again. I have to tell myself twice so I knock off the snacking.)
- Citrus products
- Spicy foods – black pepper, garlic, onions
There are a million and one diet books on acid. Basic nutrition and a list of trigger foods don’t require 200 pages or 9 editions or any special knowledge beyond what’s shared here. Dropping Acid is the only book we currently sanction as it is pretty straightforward, evidence-based, and comprehensive.
Some people will do the whole “Alkaline” diet thing to try to combat the acid. While the food choices of an “alkaline diet” are in general healthier, some of those diets have reflux trigger foods.
Management of Reflux
So we are clear, reflux a couple times a year is only annoying. Reflux that happens frequently or even consistently can end up being a problem.
Reflux symptoms must be separated from the long-term complications of reflux. Think of it like blood pressure. If your boss is giving you lip, you might have a spike in blood pressure. Elevated blood pressure over a long period can lead to a heart attack.
While we can easily remove the symptoms of reflux, we must monitor the disease (via a health professional like a GI doc) to ensure the disease isn’t manifesting into something serious.
You can go to yoga to get your momentary blood pressure down, but we must keep an eye on our heart health over a long period to ensure we don’t have the big one.
This is where my “rant” happens. It is extremely irresponsible for a “supplement expert” to tell you to treat reflux naturally without ensuring you have a GI doc looped into your plans at the least.
Traditional Reflux Treatment
Traditional treatment of reflux involves a three-step process. Think of it like a ladder.
- At the bottom rung are very short-term options to quickly resolve the symptoms right now, but has no impact on the disease itself (as evident by the real data). Tums and other antacids neutralize the gut pH right now, but quickly wear off.
- The next level are medicines called histamine 2 blockers (H2 Blockers). Pepcid, Zantac, Tagamet, etc make up this rung. They work much longer – over 8-12 hours – and can have an impact on healing the esophagus and preventing long-term disease. This is a dose-related effect though – you have to take higher doses, usually prescribed by the doc.
- The top rung holds the proton pump inhibitors (we’ll use PPIs after this, or as most of our customers call them, “the devil”). This is Aciphex, Prilosec, Nexium, Protonix, Prevacid, and whatever other copycat drug came out in the mid to late 90s. These medicines drastically shut down acid production and are the ones with the evidence to not only resolve symptoms, but treat and prevent GERD and its complications.
Reflux – It Repeats On You
Mention the word PPI and many natural-leaning reflux sufferers bring up more than just acid.
So many people are doing everything they can to avoid the medicines associated with reflux. Is this justified?
Isolated, direct cases of reflux (i.e. you just ate a punch bowl of spaghetti and marinara and downed a bottle of red) can be treated as you best see fit. Grabbing some tums, taking over-the-counter medicines, or reaching for natural products.
Reflux that happens frequently must be addressed at a “higher level” than self-care. Frequently means anything that needs treatment for 7-14 days and happens more than a few times a year.
It is completely irresponsible for an “expert” to point you towards natural treatments, away from traditional medicine, without proper monitoring and conversations with a doctor.
We can do a really good job at getting rid of symptoms. What if the acid persists in the esophagus, slowly changing those cells cancerous? We could mask the normal signs our body throws out there when it needs help.
If you don’t want traditional medicine, fine, but those suffering from GERD should have regular appointments with a gastroenterologist so they can monitor you efficiently.
PPIs
Many people who come to us absolutely hate PPIs. They have this horrible reputation as being unsafe, side effect causing, long term problems. Is this justified?
If I may rant, it is odd to me that so many “experts” in the natural products world use small studies to justify everything, all while ignoring larger, more definitive data. “Oh look, a study in 5 rats that showed apple cider vinegar at 50x normal dose reduces a specific cancer presence… Apple cider vinegar cures cancer and should be given to everyone!”
Mention the study in 100 patients where the apple cider vinegar theory was tested and showed no change in any disease state… crickets are all you hear.
The reason I bring that up is because if you dig into the data around PPIs, we can come to some solid, conservative, “middle path” conclusions about them.
Here are some myths and truths about PPIs:
TRUTH: PPIs are overprescribed. For certain, most people who are using PPIs don’t need them. This has more to do with people getting them in the hospital for “stress ulcers” and then continuing on them when they go home than it does people using PPIs for GERD.
MYTH: PPIs cause addiction. Prilosec won’t make you gamble or get hooked on smack, but using long term PPIs can cause physical dependence. This means your body’s natural acid production is shut down for so long it gets, well, fat and lazy.
It takes a while for it to “get back in shape” after PPI use, resulting in a rebound high acid state if a PPI is stopped suddenly. We recommend decreasing PPI use slowly over 4-6 weeks to prevent this from happening.
HALF TRUTH: PPIs cause fractures. PPI use will alter the absorption of calcium, magnesium, and B12. Over time, people who already have some bone disease or other compounding risk factors, can see worsening bone disease and possibly fractures. The important part to know is that the risk is insanely small.
It takes 2000 women using high dose PPI for a year to cause a single fracture. That being said, using a properly made, absorbable form of calcium and magnesium (especially) is important while on a PPI.
MYTH: PPIs cause dementia and heart disease. There’s some data floating around that links PPIs to heart problems and even dementia. Most practitioners look at this and see a possible correlation (they could be related), but know there is no definitive causation (A causes B to happen).
“You’re Just A Shill For Big Acid”
Do I get a percentage of Big Pharma stock for writing this? No. In fact, pharmacy owners get like $3 total to fill a PPI prescription, where we make way more on supplements.
My ask here is that before we get our pitchforks out for PPIs, we consider the following:
- PPIs or H2 Blockers get the job done definitively and may be needed to heal you and keep you healthy.
- The risks do NOT outweigh the benefits, especially when used responsibly for only short term.
- You decide what “short term” is with a health professional, not an internet doctor (or pharmacist for that matter).
- Medicines are far cheaper than supplements
- Doing the self-care stuff like diet changes, avoiding trigger foods, and just being an anti-acid reflux crusader will only take you so far sometimes. Sometimes reflux persists despite our best efforts, and we may have to look to medical therapy and that’s all there is to it.
That’s the end of my hardcore rant portion of the rant, beyond my normal railing against quality in the supplement industry. I’m not asking anyone to take the traditional medicines, I’m just saying that the middle path applies here more than most places.
Supplements To Support Gut and Esophageal Health
You’ve eliminated all possible trigger foods, even chocolate. You chew 58 times before swallowing, taking the flavor out of your food and joy out of eating, making it a horrific chore. What other self-care options do we have to keep our gut healthy and potentially quell symptoms of reflux? We have lots!
Probiotics – the key to a healthy gut. One strategy is to open the capsule and mix it with something to “expose” the upper GI tract to some of the flora. Won’t hurt.
Digestive Enzymes – helping break down foods may be a key to reducing reflux symptoms. Most people don’t need digestive enzymes, but some have reported successful GI support using them. Must be used 30 minutes before a meal or snack.
Calcium/Magnesium – for patients on a PPI, supplementing with absorbable forms of calcium and magnesium are important. Calcium Hydroxyapatite is the only form to make an impact on bone, and magnesium chelates will absorb better.
DGL (deglycyrrhized licorice) – licorice has potential impacts on blood pressure, but if it is deglycyrrhized, those risks are almost eliminated. DGL supports a healthy GI tract via potential anti-inflammatory properties and an overall soothing of a roughed-up GI tract.
Aloe – Aloe has been used for centuries for its role in supporting the GI tract. Anecdotal evidence suggests it supports healthy inflammation in the GI tract.
Zinc Carnosine – carnosine is an amino acid with important roles in the healing epithelial cells and zinc is used by the body in wound healing. Some believe zinc carnosine is an option for repairing damage done by acid reflux.*
Protein – One of our Vital 5, protein is a crucial nutritional component to be healthy. We have a special protein and nutritional shake mix that also has vitamins, minerals, and herbs that support GI health. Sometimes it’s best to take a break from our harsh diet and eat more bland options until the reflux passes.
B Vitamins – B12 and other vitamins may be necessary, especially if someone is on a PPI as it reduces the absorption of B12 from our diet. A good option is homocysteine support.
Solid options for someone looking to support healthy acid levels:
Oh My GERD!
Millions of people suffer from reflux on a daily basis to varying degrees. As per the internet, all traditional medicines for reflux will cause your head to fall off, your pets to go feral, and your kids will start hiding the remote – all evil stuff.
We want you to make the best, informed decision around management of reflux. Do everything in your own power to reduce reflux risks – avoid trigger foods, eat slower while sitting, chew thoroughly, have frequent, small meals, avoid high-fat meals, and don’t eat before bed or naps (who naps??).
Use properly made supplements to support your GI health like probiotics and digestive enzymes.
Most importantly, don’t go it alone. Make your doctor aware of frequent reflux symptoms. Be open to a short course of traditional meds, even PPIs.
Be aware of their REAL shortcomings. Use properly made calcium, magnesium, or B12 to reduce your complication risks down to almost nothing.
If you still are dead set against the meds if a professional recommends it, have an honest discussion of risks and expectations. As long as you have the conversation.
Just trying to keep it real…

Neal Smoller, PharmD
Owner, Pharmacist, Big Mouth